Percussion, a fundamental method of clinical examination, involves the gentle tapping of a patient’s body with the examiner’s fingers.
This technique generates specific sounds, revealing invaluable information about underlying tissues.
In this comprehensive guide, we dig into the world of percussion, covering its definition, the sounds it produces, and the critical role played by the pleximeter and plexor finger.
Furthermore, we will explore the vibrations felt during percussion and their diagnostic significance.
Table of Contents
ToggleDEFINITION OF PERCUSSION
Percussion, in the context of clinical examination, involves tapping or striking a part of the body with the fingers to produce specific sounds and assess the underlying tissues.
This method offers vital diagnostic information by producing audible vibrations within the body, enabling the examiner to both hear and feel the resulting vibrations in their fingers caused by the impact.
So, there are two main aspects:
- Hearing Vibrations: When you tap the body, it makes a sound because of vibrations inside. You can hear this sound.
- Feeling Vibrations: At the same time, the tap creates vibrations that you can feel through your fingers.
UNDERSTANDING PERCUSSION SOUNDS
The sound you hear during percussion depends on two things:
- How Much Tissue Vibrates: The sound quality changes based on how much tissue vibrates from the tap. A harder tap makes more tissue vibrate, altering the sound.
- The Kind of Tissue: The type of tissue that gets tapped also matters. Different tissues in the body vibrate at different rates, affecting the sound you hear.
POWER OF THE TAP
How hard you tap is important.
A stronger tap reaches deeper tissues, which vibrate differently.
So, the sound changes. This means the sound you hear is unique to an organ when you tap it just right.
DISCOVERING TISSUE TRAITS
By tapping with a known force, doctors can learn about the physical qualities of the organ’s tissues.
This helps predict what the tapping will sound like.
Percussion, along with other exams like feeling and listening, gives doctors a complete set of tools to check for many medical issues.
This method, based on sound and vibrations, has been used in medicine for a long time and is still very useful today.
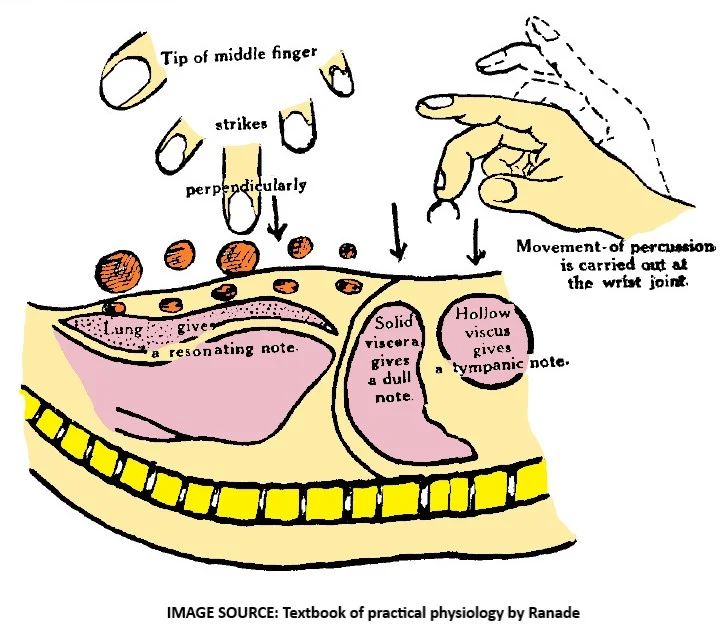
TYPES OF THE PERCUSSION SOUNDS
The art of percussion provides crucial insights into the body’s internal structures.
Through precise tapping or striking of the body’s surface, medical professionals can get valuable information about various tissues.
This technique classifies these tissues and the resulting percussion notes into three primary categories:
Tympanic (Hollow Viscera)
- These are organs that contain gas within their cavities.
- When you percuss such organs, the resulting note is reminiscent of a musical tone.
- It’s as if the body is revealing its inner melody.
- The term “tympanic” is used to describe this specific sound.
Resonant (Visceral Tissue with Air Trapped)
- Organs like the lungs, where air is confined within tiny compartments, produce a distinct resonant note.
- This note is characterized by being low-pitched and usually quite loud.
- It possesses the ability to travel a distance, making it easily detectable even from afar.
Dull (Solid Viscera)
- Solid viscera, which are typically composed of soft, fleshy material, fluids, or hard bones, elicit a note known as “dull” during percussion.
- This note is high-pitched, of short duration, and can only be heard when you’re in close proximity to the organ being examined.
It’s important to note that within the human body, many organs are composed of a mixture of various tissues.
In such cases, you can expect to hear intermediate types of percussion notes as a result.
Furthermore, when different types of tissues are arranged in distinct layers within an organ, the character of the note can vary depending on the strength of the percussion impact.
- For instance, if gas is present in deeper structures of an organ, you’ll likely hear a tympanic note only when percussing with significant force. In contrast, light percussion may produce a dull note in these areas.
- On the other hand, when lung tissue covers the heart superficially, gentle percussion may yield a resonant note, while stronger percussion may result in a dull note.
So, in the world of percussion, the sounds tell a rich and subtle story about what’s happening inside the body, offering healthcare professionals valuable clues in their diagnostic journey.
PLEXIMETER AND PLEXER FINGER
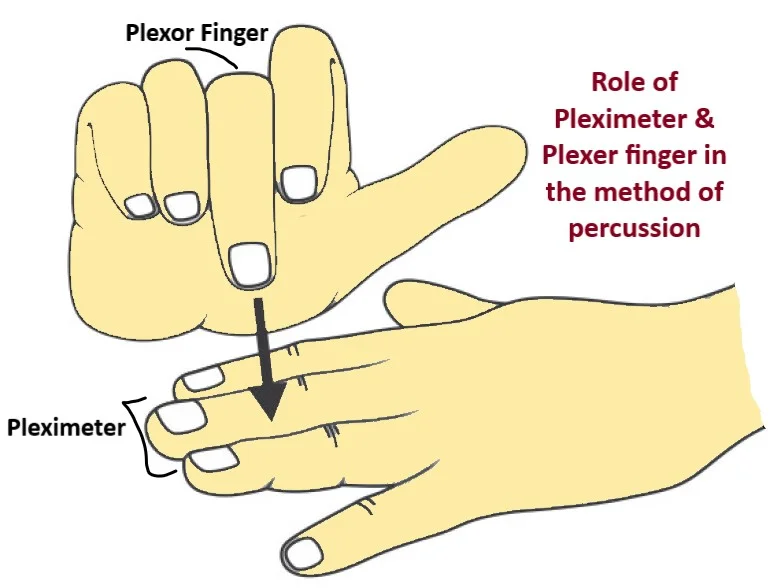
Before proceeding to explore percussion techniques, it’s vital to understand the roles of two essential components: the pleximeter and the plexor finger.
Pleximeter
- This is an object or surface placed on the body area under examination. Its main job is to provide a stable surface for the percussion strike, enabling sound wave generation within the body.
- Direct contact between the pleximeter and the body’s surface is vital for accurate results.
- Materials like the middle finger of the left hand, percussion hammers, or flat objects made of wood, ebonite, or plastic can serve as pleximeters. However, using fingers is often preferred for precision.
- Artificial plexors and pleximeters usually don’t offer significant advantages and can introduce errors if used incorrectly.
Plexor Finger
- This is the finger used to deliver the percussion stroke. While any finger can theoretically be used, the middle finger of the right hand is the common choice.
- The middle finger’s length and simplicity make it ideal for consistent, strong strikes.
- During percussion, the middle finger’s tip strikes the surface being examined perpendicular to it, with wrist joint flexion and extension driving the movement.
- Other fingers and hand muscles mainly stabilize the middle finger, creating a steady framework. This minimizes elbow movement, keeping the shoulder joint still.
- After the percussion stroke, quickly lift the plexor finger to prevent damping vibrations.
In essence, the pleximeter provides a stable surface for percussion, ensuring continuous contact with the body area of interest.
The plexor finger, typically the right middle finger, delivers controlled and consistent percussion strokes.
HOW TO PERCUSS?
Step 1: Finger Selection
- Choose your middle finger, ideally from your right hand. Its length and reduced agility make it ideal for delivering uniform, powerful strikes.
Step 2: Finger Placement
- Use the tip or pad of your middle finger.
- Strike the surface at a right angle to the area you’re examining.
- Keep your arm alongside your body.
- Generate the percussion movement by flexing and extending your wrist joint.
Step 3: Stabilization
- Engage the muscles in your hand and other fingers to stabilize the middle finger.
- Ensure minimal elbow movement and keep the shoulder joint still.
Step 4: Applying Force
- Adjust the force based on the organ you’re examining.
- Lift your finger immediately after striking to avoid dampening vibrations.
Direct vs. Indirect Percussion
Step 5: Direct Percussion
- Use direct percussion when examining hard structures like bones or exploring deeper tissues.
- Expect resonant sounds as tissues just below the surface resonate.
Step 6: Indirect Percussion
- For indirect percussion, place your left hand’s middle phalanx on the surface to be examined.
- There should be no airspace between the body surface and your finger.
- Keep other left-hand fingers separated to avoid contact with the surface.
The Technique of Percussion
Step 7: Percussion Direction
- Always move from a resonant or tympanic area to a dull area.
- Percuss perpendicular to the border.
Step 8: Special Considerations
- Note that when percussing bones, the entire bone acts as a pleximeter. Smaller areas within the bone’s surface may not be detectable during percussion.
VIBRATIONS FELT DURING PERCUSSION
When performing percussion, the vibrations felt by the examiner’s pleximeter finger provide valuable information about the underlying tissues.
This tactile sensation or resistance to percussion can be broken down into several key points:
Perception of Vibrations
Following the percussion stroke, the pleximeter finger perceives the vibrations generated within the body.
These vibrations are crucial for assessing the characteristics of the examined area.
Differences in Frequencies
The pleximeter finger has the remarkable ability to detect variations in the frequencies of these vibrations.
This means it can distinguish between different types of tissues based on the frequency of vibrations.
Duration of Vibrations
Additionally, the pleximeter finger can perceive differences in the duration of vibrations.
Some tissues may produce shorter, quicker vibrations, while others create longer, sustained ones.
Sensitivity vs. Hearing
Interestingly, the examiner’s ability to perceive these vibrations through touch is often more precise than what can be recognized by the ear alone.
This tactile sensitivity allows for a detailed assessment of tissue characteristics.
Descriptive Terminology
Based on the resistance felt by the fingers, various terms are used to describe the examined tissue.
These terms include soft, pliable, yielding, tense, hard, thudding, metallic, stony, and more.
In summary, during percussion, the pleximeter finger acts as a valuable sensor, detecting vibrations in tissues and providing insights into their composition and properties.
This tactile perception complements traditional auditory assessment and enables a comprehensive evaluation of the examined area.
CONCLUSION
Percussion, with its ability to produce audible vibrations within the body, offers healthcare professionals a unique way to assess internal structures.
The distinct sounds produced during percussion guide clinicians in categorizing tissues and diagnosing medical conditions.
By understanding the art of percussion, including finger selection, techniques, and the importance of the pleximeter and plexor finger, medical practitioners can harness this age-old method to enhance their diagnostic capabilities and provide comprehensive patient care.
FREQUENTLY ASKED QUESTIONS
- What is percussion in clinical examination?
- Percussion is a medical technique where a healthcare professional gently taps a patient’s body with their fingers. It’s used to produce specific sounds and gather vital information about the body’s internal tissues.
- Why is percussion important in healthcare?
- Percussion helps doctors assess internal structures by creating audible vibrations within the body. These vibrations can be both heard and felt by the examiner, providing valuable diagnostic clues.
- What are the two main aspects of percussion?
- Percussion involves both hearing and feeling vibrations. When you tap the body, it produces a sound due to internal vibrations, and at the same time, you can feel these vibrations through your fingers.
- How do the sounds in percussion work?
- The sounds during percussion depend on how much tissue vibrates and the type of tissue being tapped. Harder taps create more tissue vibration, altering the sound. Different tissues vibrate at varying rates, affecting the sound heard.
- Why does the strength of the tap matter in percussion?
- The strength of the tap is crucial because it determines how deep the tissues are reached. Deeper tissues vibrate differently, resulting in unique sounds that can help diagnose specific organs.
- Can you describe the types of percussion sounds in detail?
- Certainly! There are three primary types of percussion sounds:
- Tympanic: This sound is reminiscent of a musical tone and is produced by organs containing gas within their cavities.
- Resonant: Organs like the lungs, with air confined in tiny compartments, produce a low-pitched, loud sound that can travel a distance.
- Dull: Solid viscera, such as soft tissues, fluids, or bones, produce a high-pitched, short-duration note heard only in close proximity to the organ being examined.
- What role do the pleximeter and plexor finger play in percussion?
- The pleximeter is an object or surface placed on the body under examination to provide a stable surface for percussion. The plexor finger, often the right middle finger, delivers controlled and consistent percussion strokes.
- How do you perform percussion effectively?
- Percussion involves specific steps, including selecting the right finger, striking the surface at a right angle, and stabilizing your hand to minimize elbow movement. The force applied depends on the organ being examined.
- What’s the difference between direct and indirect percussion?
- Direct percussion involves tapping hard structures or deeper tissues, resulting in resonant sounds. Indirect percussion is performed by placing the left hand’s middle phalanx on the surface to be examined and is used for differentiating between resonant and dull areas.
- What can vibrations felt during percussion reveal about tissues?
- The vibrations felt by the examiner’s finger provide insights into tissue characteristics, including differences in frequency, duration, and tactile sensitivity. This information complements traditional auditory assessment.
- How can healthcare professionals’ benefit from mastering percussion techniques?
- Percussion, when understood and applied correctly, enhances diagnostic capabilities. It provides a unique way to assess internal structures, categorize tissues, and diagnose medical conditions, contributing to comprehensive patient care.




Leave a Reply