This post is about the Phases of Menstrual cycle and its regulation.
Graafian follicle and Corpus Luteum are also included at the conclusion of this post.
So, let’s get started…
Table of Contents
ToggleDEFINITION OF MENSTRUAL CYCLE
The Monthly cycle of changes in the ovaries and the uterine lining (endometrium), starting with the preparation of an egg for fertilization.
- Its repeated at an average interval of about 28-30 days.
- The cycle of events from one menstruation till next one is known as menstrual cycle.
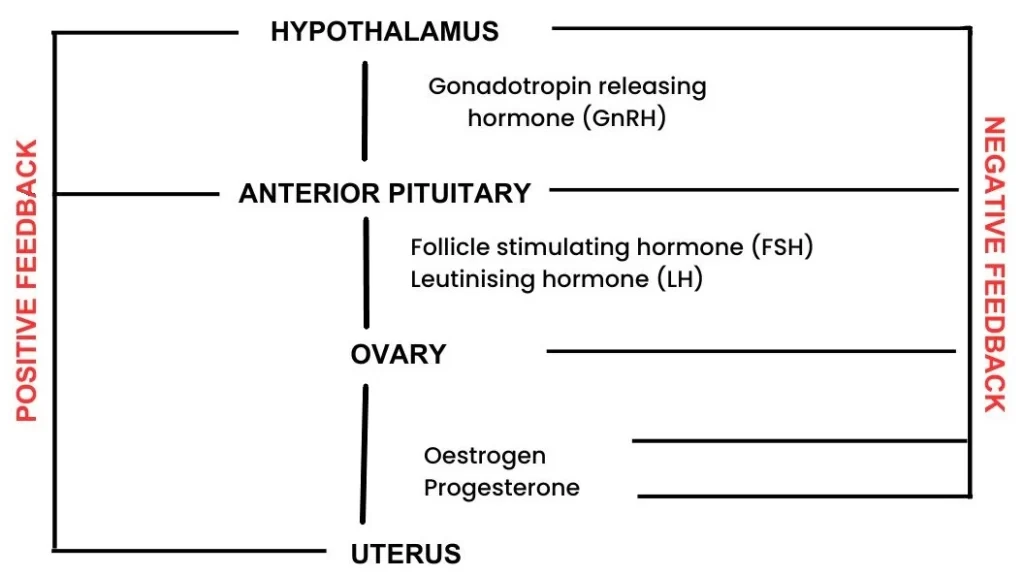
HORMONES OF MENSTRUAL CYCLE
1.ANTERIOR PITUITARY HORMONES
- Luteinizing hormone (LH)
- Follicle stimulating hormone (FSH)
2.OVARIAN HORMONES
- Oestrogen
- Progesterone
FUNCTIONS OF HORMONES
LH
- Surge (outpouring) causes ovulation.
- Development of corpus luteum.
- Stimulates progesterone secretion.
FSH
- Stimulates follicular growth.
- Stimulates oestrogen secretion from developing follicle.
OESTROGEN
- Development of endometrium.
- Stimulates LH secretion (follicular phase).
- Inhibits LH & FSH (luteal phase).
PROGESTERONE
- Thickening of endometrium.
- Inhibits LH & FSH (luteal phase)
MENSTRUAL CYCLE PHASES
Changes in level of Anterior pituitary hormone & Ovarian Hormones causes changes in ovary & uterus, which results in different phases.
Menstrual cycle can be divided into 4 phases
1.Menstrual phase 1-4
2.Follicular (oestrogen)phase 5-13
3.Ovulation 13-16
4.Luteal (progesterone)phase 16-28
How long does a period (Menstrual cycle) last?
A normal healthy female may have 4 to 7 days of menstrual bleeding.
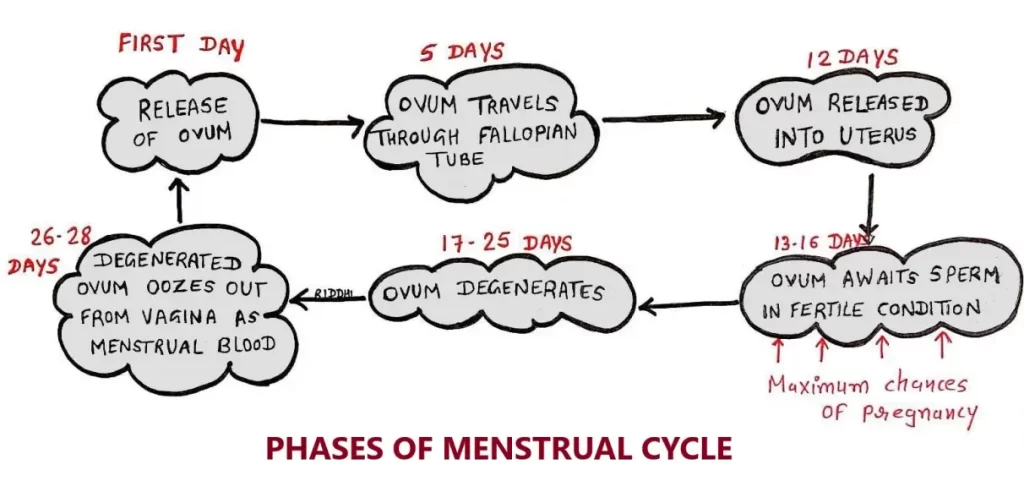
1. MENSTRUAL PHASE/ SECRETORY PHASE 1-4
- Starts with menstruation.
- Discharge of bloody fluid containing endometrial cells, Glandular secretions & blood cells.
- Reason is due to breakdown of endometrial lining of uterus & its blood vessels.
- Because of strong vasoconstriction & proteolytic activity, layer of endometrial tissues dies & is discharged during menstrual bleeding.
- Endometrium becomes very thin, but due to low oestrogen levels, hypophysis secretes more FSH.
- FSH stimulates oestrogen secretion.
- Oestrogen causes proliferation in endometrial basal layer.
2. FOLLICULAR PHASE (OESTROGEN)/ PROLIFERATIVE PHASE 5-13
- Because of the rise in follicle stimulating hormone (FSH) level during first day of cycle, several ovarian follicles are stimulated.
- Follicles compete with each other for development.
- Follicle mature into Graafian follicle (described at the end of this post).
- As they mature, follicles secrete increasing amount of oestrogen, which thickens new functional layer of endometrium in uterus.
- As in this phase endometrium regenerates through proliferation, this phase is also known as Proliferative phase.
- Oestrogen also stimulates crypts in cervix to produce fertile cervical mucus.
- At end of this phase ovulation occurs.
3. OVULATION 13-16
- During follicular phase, Oestrogen suppresses production of Luteinizing Hormone (LH) from pituitary gland.
- When ovum is nearly matured, levels of Oestrogen reach a threshold above which they stimulate production of LH (Positive feedback mechanism).
- Both LH & FSH attains a peak value called LH SURGE.
- Release of LH matures ovum & weakens the wall of follicle in ovary, causing Graafian follicle rupture & release of ovum.
- After being released from ovary, the ovum stays in fallopian tube.
4. LUTEAL PHASE (PROGESTERONE) 16-28
- Graafian follicle transforms as Corpus Luteum (described at the end of this post).
- Corpus Luteum is a solid body formed in ovary, after ovulation.
- Corpus Luteum secrets significant amount of Progesterone, which plays a vital role in making the endometrium receptive to implantation of blastocyst.
- High levels of Oestrogen & Progesterone suppress production of FSH & LH that Corpus Luteum needs to maintain itself.
- In absence of fertilisation, corpus luteum degenerates.
- Falling levels of Progesterone degenerates endometrium lining, trigger menstruation & beginning of new cycle.
SIGNS OF MENSTRUAL CYCLE
- Bleeding from vagina is the primary sign of menses.
- Some women have other symptoms around the time of menses including CRAMPING, BLOATING, SORE BREASTS, FLUID RETENTION, MOOD SWINGS & IRRITABILITY, WEIGHT GAIN, DIARRHOEA, CONSTIPATION, HEADACHE & FATIGUE.
- PMS (Premenstrual Syndrome) usually occurs one or two weeks before menstruation.
MENARCHE
- A woman’s first menstruation.
- Typically occurs around age of 12.
- Occurrence depends on overall health & diet.
MENOPAUSE
- End of women’s reproduction phase.
- Commonly occurs between age 45-55 depends on genetics.
MENSTRUAL DISORDERS
1. Menorrhagia:An excessive uterine bleeding.
2. DUB: Excess, prolonged, frequent bleeding.
3. Oligomenorrhea: Uterine bleeding at interval of 35 days & 6 months.
4. Amenorrhoea: No menses for at least 6 months.
5. Anovulation: Failure of ovary to release ova for more than 3 months.
OVARIAN CHANGES DURING MENSTRUAL CYCLE/ OVULATION PERIOD
INTRODUCTION
- Process by which Graafian follicle in ovary ruptures and ovum is released into abdominal cavity.
- Occurs on 14th day of menstrual cycle in a normal cycle of 28 days.
- The ovum, which is released into the abdominal cavity, enters the fallopian tube through fimbriated end of tube.
- Usually, only one ovum is released from any one of the ovaries.
- LH is responsible for ovulation.
PROCESS OF OVULATION
- Prior to ovulation, large amount of LH is secreted (luteal surge).
- This causes changes in the Graafian follicle leading to ovulation.
STAGES OF OVULATION
1. Graafian follicle moves towards the periphery of ovary.
2. New blood vessels are formed in ovary by actions of LH & Progesterone.
3. These blood vessels protrude into wall of follicle.
4. This increases blood flow to follicle.
5. Now, Prostaglandin is released from granulosa cells of follicle.
6. It causes leakage of plasma into follicle.
7. Just before ovulation follicle swells and protrudes against capsule of ovary. This protrusion is called stigma.
8. Then, progesterone activates the proteolytic enzymes present in cells of theca interna.
9. These enzymes weaken follicular capsule & cause degeneration of Stigma.
10. After about 30 minutes, fluid begins to ooze from follicle through Stigma.
11. It decreases size of follicle causing rupture of stigma.
12. Now, ovum is released from follicle along with fluid & plenty of small granulosa cells into abdominal cavity.
GRAAFIAN FOLLICLE
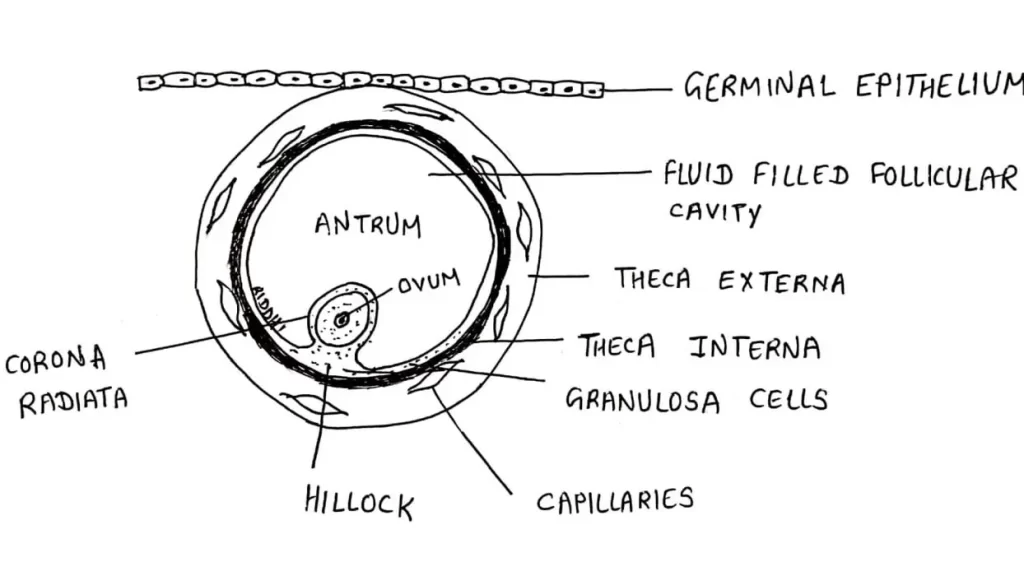
- Graafian follicle is a mature ovarian follicle with maturing ovum.
- It is named after Dutch physician and anatomist, Regnier De Graaf.
Changes taking place during development of graafian follicle
1) Size of follicle increases to about 10 to 12 mm, It extends through the whole thickness of ovarian cortex.
↓
2) At one point, follicle intrude on tunica albuginea and protrudes upon surface of ovary. This protrusion is called stigma.
At stigma, the tunica albuginea becomes thin.
↓
3) Follicular cavity becomes larger and distended with fluid.
↓
4) Ovum attains maximum size.
↓
5) Zona pellucida becomes thick.
↓
6) Corona radiata becomes prominent.
↓
7) Small spaces filled with fluid appear between cells of germ hill, outside the corona radiata.
↓
8) These spaces weaken attachment of ovum to follicular wall.
↓
9) Theca interna becomes prominent. Its thickness becomes double with the formation of rich capillary network.
↓
10) On the 14th day of menstrual cycle, graafian follicle is ready for the process of ovulation.
CORPUS LUTEUM
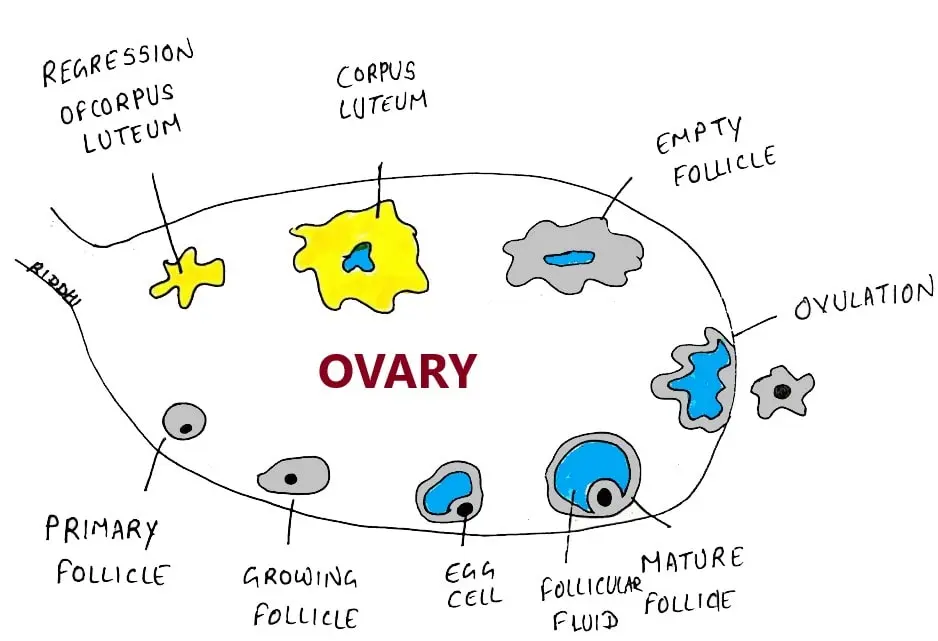
- Glandular yellow body.
- Developed from ruptured Graafian follicle after release of ovum.
- It is also called Yellow body.
DEVELOPMENT
1. Soon after rupture of Graafian follicle and release of ovum, follicle is filled with blood. (Corpus Hemorrhagicum).
2. The blood clots slowly. Corpus hemorrhagicum does not degenerate immediately. It is transformed into corpus luteum.
3. Follicular cavity closes gradually by healing of wound. Blood clot is gradually replaced by a serous fluid containing fibrin.
4. Corpus luteum obtains a diameter of 15 mm and remains in the ovary till end of the cycle.
STRUCTURE
- LUTEINIZATION: In Corpus Luteum, granulosa cells and theca interna cells are transformed into lutein cells called Granulosa Lutein Cells and Theca Lutein Cells.
- Granulosa lutein cells contain fine lipid granules & yellowish pigment.
- Granules give characteristic yellow colour to corpus luteum.
- Theca lutein cells contain only lipid granules and not yellow pigment.
- Follicular cavity is greatly reduced with irregular outline.
- It is filled with serous fluid and remnants of blood clots.
FUNCTIONS
1.Secretion of hormones: It secretes large quantity of Progesterone and small amount of Oestrogen.
2.Maintenance of pregnancy: Hormones are secreted by corpus luteum during pregnancy for about first 3 months of pregnancy.
FATE
Depends upon whether Ovum is fertilized or not.
If ovum is Not Fertilized,
- It degenerates into corpus luteum menstrualis.
- The cells decrease in size and corpus luteum becomes smaller and involuted & is transformed into a whitish scar called corpus albicans.
- The process by which corpus luteum undergoes regression is called luteolysis.
If ovum is Fertilized,
- Pregnancy occurs, corpus luteum persists and increases in size.
- It attains diameter of 20 to 30 mm & transformed into corpus luteum of pregnancy.
- It remains in ovary for 3 to 4 months & secretes large amount of Progesterone with small quantity of Oestrogen to maintain pregnancy.
- After 3 to 4 months, placenta starts secreting these hormones and corpus luteum degenerates.
