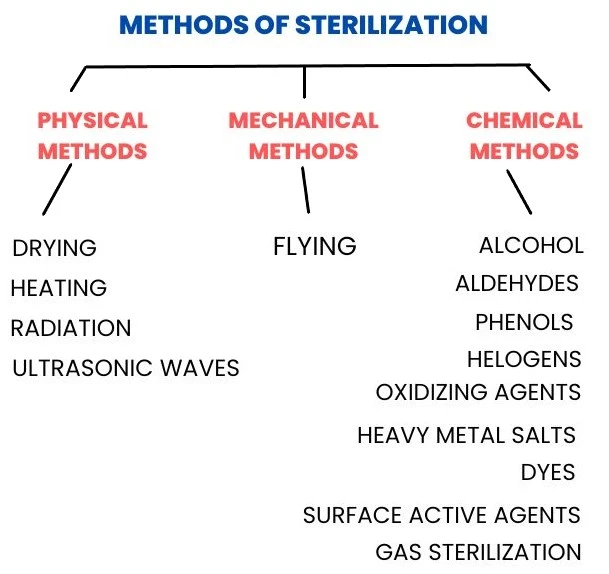
The methods of sterilization is a very vast subject so I have divided it into three parts.
This post is mainly focused on the Physical methods of sterilization.
The scientific ways to control microbial growth began just about 100 years ago.
Let’s recall Louis Pasteur’s discoveries which caused microbiologists to believe that microbes might be the cause for the diseases.
In mid-18th century, the English physician Joseph Lister and Hungarian physician Ignaz Semmelweis were the first who found it necessary to develop the methods to control the growth of microorganisms before medical procedures.
Why these methods are necessary?
Before 18th century, Hospital acquired infections (HAI/ HCAI- Health Care Associated Infections) were the cause of death in 10% of surgical cases & up to 25% deaths of delivering mothers.
Then what did the scientists do to solve these problems?
From many decades, scientists have developed different types of Physical, Chemical and Mechanical methods to control growth of microorganisms.
Factors that affect the effectivity of sterilization treatment:
- Number of microbes- Larger the number of microbes, longer will be the time to eradicate.
- Environmental conditions- Hot or warm environment provides better results for most of the disinfectants.
- Organic matters like blood, vomitus, feces etc. may inhibit the action of disinfectants.
- Nature of suspension medium in which microbes lives also affects.
- Time of exposure- More exposure time causes more positive results.
- Characteristics of microorganisms.
- Concentration of chemical agents.
[Note: Before we go through all these methods do revise some important terminologies given as a reference in the table at the end of this post.]
So, how these sterilizing agents work?
- Alteration in permeability of bacterial cell membrane-
- Damage to the plasma membrane of bacterial cell causes leakage of cellular content into the surrounding medium and affects the growth of a cell.
- Damage to proteins & nucleic acids-
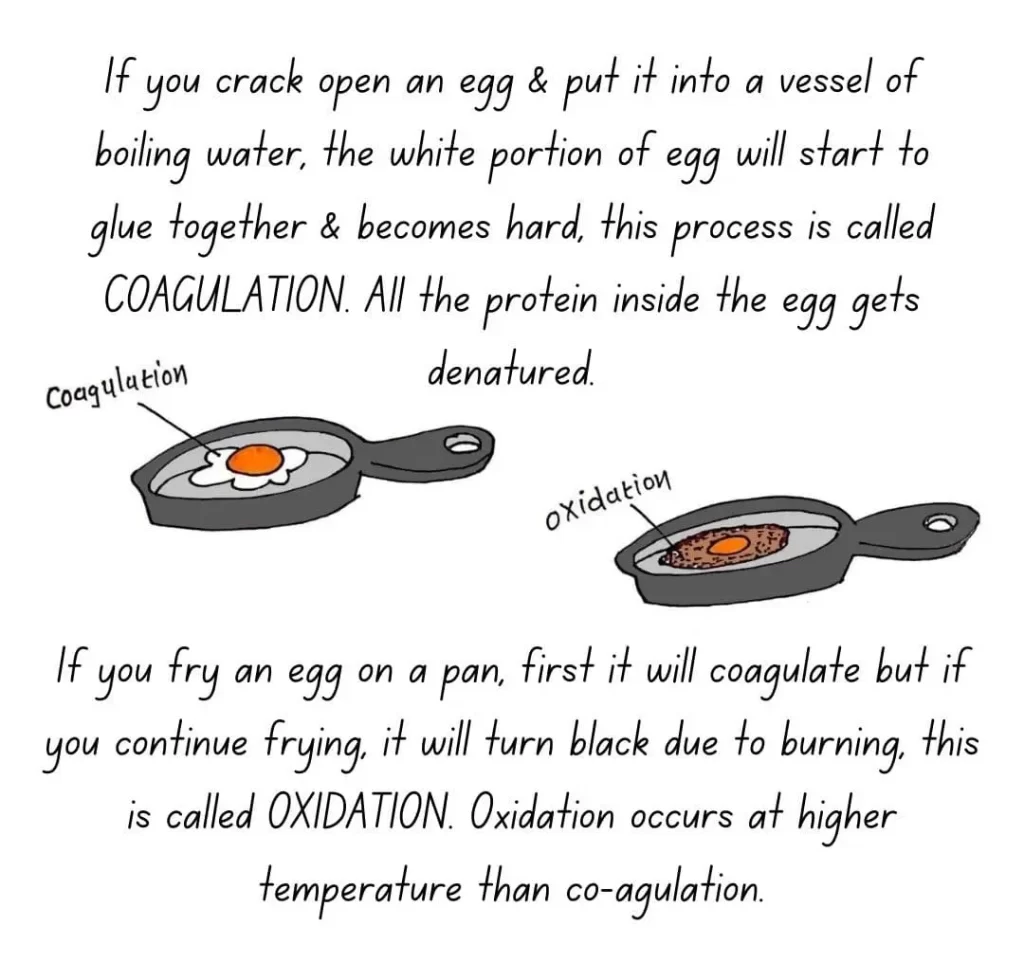
- Heat and certain chemicals break the Hydrogen bonds of primary Proteins (Enzymes) and denatures them.
- Protein denaturation means it loses their structure so, it cannot perform the functions it normally does.
- Once denatured, they can’t break the molecules down and neither fasten the processes.
- Damage to the DNA & RNA of cell ends the replication and normal metabolic processes.
What method we should choose?
Before selecting the method, we should consider the effects of that particular method because,
- Some vitamins or antibiotics might become inactive due to heat.
- Repetitive heating procedures may damage many hospital and laboratory utensils like rubber, plastic or latex.
Table of Contents
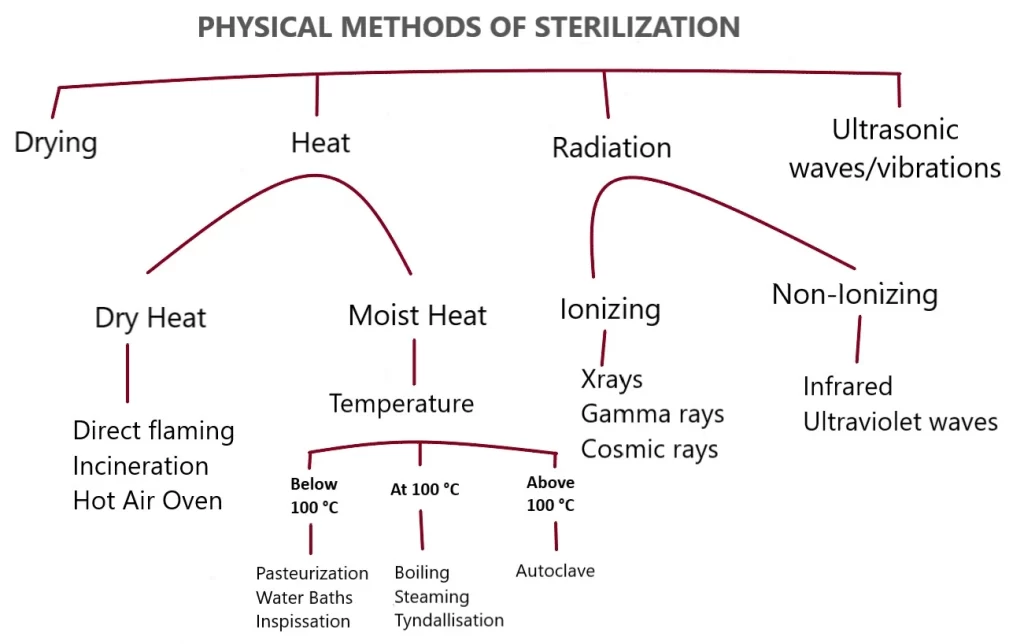
TogglePHYSICAL METHODS OF STERILIZATION
Sterilization using physical methods is as old as the stone age.
Example– Drying (desiccation) and salting (osmotic pressure) to preserve foods.
(You might have seen your mother and grandmother making pickles and wafers at home by soaking it in salt overnight before drying in sunlight to store them for over the year).
1. DRYING

- Adequate moisture is necessary for organisms to grow.
- Semple and Grieg observed that in India, bacilli causing typhoid dies within 2 hours after sun exposure. But, may survive in dark place for more than 6 days.
- Sunlight provides considerable bactericidal effects due to UV and Heat rays.
- Therefore, drying causes damage to many bacteria.
- But, Bacterial spores and some species of viruses may survive.
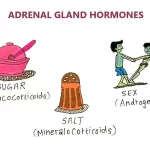
2. HEAT
- Most reliable.
- Commonly used method.
- Because, heat can destroy Proteins inside the organisms which is known as denaturation.
- Two types- Dry heat and Moist heat.
1. DRY HEAT
Done by Direct flaming, Incineration and Hot Air Oven.
Direct flaming
- Items to be sterilized are directly held in the flame of Bunsen burner for short or long time.
- Commonly used to sterilize small glass or metal utensils used in laboratories and pharmaceutical industries.
- Advantage- Non time consuming and economical.
Incineration
- Biological wastes like placenta, used dressings and organs etc. are converted into ash or flue gas by applying very high temperature (870°C-1200°C ).
- Advantage- Volume of material decreases up to 90%.
- Disadvantage- Total destruction, high construction and costly.
[Read in detail at Methods of sterilization part 3].
Hot Air Oven
- It is an electric chamber, made up of stainless steel from inside.
- Glassware (syringes, petri dishes, test tubes etc.), surgical instruments (scalpels, forceps etc.) or chemicals can be sterilized.
- Most widely used method.
[Read in detail at Methods of sterilization part 3].
Advantages of dry heat sterilization
- Relatively low cost.
- Dry heat penetrates materials.
- Non-toxic and safe to environment.
- Non-corrosive for metal and sharp instruments.
Disadvantages of dry heat sterilization
- Time consuming due to rate of heat penetration and killing of microbes is low.
- High temperatures are not suitable for many materials.
2. MOIST HEAT
Kills microorganisms by coagulation of cellular Proteins (denaturation).
- Temperature below 100°C – By Pasteurization, Water baths and Inspissation.
- Temperature at 100°C – By Boiling, Steaming and Tyndallisation.
- Temperature above 100°C – By Autoclave.
Temperature below 100°C
Pasteurization
- Louis Pasteur found a practical method to prevent microbial control by applying mild heat sufficient to kill microbes.
- Pasteurization is the treatment for elimination of harmful pathogens from milk, yogurt, beer, fruit juices or other packaged food (mostly liquid).
- All non-sporing microbes like Mycobacteria, Brucellae, Salmonella are destroyed.
- Coxiella Burnetii may survive due to heat resistance.
[Read in detail at Methods of sterilization part 3].
Inspissation
- Instrument used- Inspissator.
- Inspissate means to make thick by evaporation.
- In this process, equipments are heated for consecutive 3 days for 30 minutes at 80-85°C.
- In first exposure, all vegetative forms of microbes get killed.
- Then, in following heating intervals remaining spores germinate into growing forms, which also gets killed by further heating.
Water bath
- It is a vessel/ container that maintains a constant temperature of water.
- Used to sterilize serum, vaccines or body fluids.
- Used to prepare culture media.
- Used In coagulation studies.
- Used to warm chemical reagents.
Temperature at 100°C
Boiling
- Boiling is a process by which liquid converts into vapor when heat is applied up to boiling point.
- Boiling of utensils for at least 15-20 minutes can kill most of the growing bacteria, fungi and many viruses but spores can survive.
- Very simple, most suitable for domestic purpose.
Steaming
- Steam is an effective carrier of thermal energy and acts as a sterilant.
- Very simple and effective.
- Equipments or media need to be sterilized are exposed to steam at atmospheric pressure for up to 90 minutes.
- Most vegetative forms of bacteria get killed except heat resistant and spore forms of bacteria.
Tyndallisation/ Intermittent sterilization
- Named after the inventor John Tyndall.
- The principle is similar to Inspissation, difference is that the temperature here is 100°C (instead of 80°C like Inspissation).
- Process- Steam exposure of 100°C for 30 minutes for 3 consecutive days.
- Used to sterilize eggs, serum or sugar rich media.
Temperature above 100°C
Autoclave
- It is an instrument functions similar to pressure cooker used for sterilization processes.
- Auto means self and clavis means key which suggests a “Self-locking device”.
- Principle- When pressure of gas increases, the temperature of gas also increases equally.
- Process- Saturated steam is allowed to penetrate under pressure through material to be sterilized for 15 minutes at 121°C.
[Read in detail at Methods of sterilization part 3].
3. RADIATION
- In this process, various effects may occur on cell depending up on wave length, intensity and duration.
- Two types of radiations are available- Ionizing and Non-Ionizing.
Ionizing
- Shorter wave length and high in energy.
- Rapidity in action.
- X-rays, Gamma rays and Cosmic rays are the examples.
- Destructs DNA without rise of temperature.
- Best method because it destroys endospores and vegetative both forms of bacteria.
- Used in medical, dental and pharmacological supplies.
Non-Ionizing
- Longer wave length & low in energy.
- Infrared and Ultraviolet waves are the examples.
- Have some limitations because they cannot penetrate glass, films water etc.
- But can damage DNA.
4. ULTRASONIC WAVES/ VIBRATIONS
- High frequency of Ultrasound waves can damage bacterial cells.
- Not very reliable and not widely used.
Hope you enjoyed learning the Physical methods of sterilization but wait, we are not done yet because Mechanical and Chemical methods of sterilization also need to be explained which you can find in the post METHODS OF STERILIZATION PART 2.
Don’t forget to read some of the important physical methods like Autoclave, Hot air oven, Incineration and Pasteurization in a separate post here METHODS OF STERILIZATION PART 3.
REFERENCE TERMINOLOGIES
- Sterilization– The process which can remove or destroy all the living microorganisms.
- Sterilant– An agent used to sterilize, like physical or chemical etc.
- Commercial Sterilization (CS)– It is the thermal process of heating the food with 121 moist heat for 15 minutes before sealing the food in containers.
- Disinfection– The process which can kill (destroy) the harmful microorganisms.
- Sepsis– Sepsis is a Greek word which means “Decay or Putrid”. Which indicates bacterial contamination.
- Aseptic– Free from pathogens.
- Pathogens– A bacterium, fungi, virus or other microorganism that can produce disease.
- Antisepsis– When disinfection treatment is done on living tissues, it is called antisepsis. Chemical used is called Antiseptic or Disinfectant.
- Degermining– Removal of microbes in a limited area, mostly soap and water or alcohol-soaked swabs are used.
- The treatment / process in order to kill the microbes have the Suffix -Cide which means “to kill”.
Examples: Biocide/ Germicide- Kills microorganisms.
Fungicide- Kills fungi.
Virucide- Kills viruses. - The treatment which inhibit the growth and multiplication of bacteria have the Suffix -Stat or -Stasis which means “to stop or to steady”. Example: Bacteriostatic.
- Nature of disinfectant–
- Ability to kill microorganisms.
- Rapidity of action.
- Ability to act in presence of organic substances.
- Residual activity.





Thanks for the topic it was worth reading