Hello again, this post is an extension of methods of sterilization part 1 where you learnt about physical methods of sterilization.
This post is focused more towards the benefits of students as we are going to discuss a few of the physical methods in detail here.
Table of Contents
TogglePASTEURIZATION
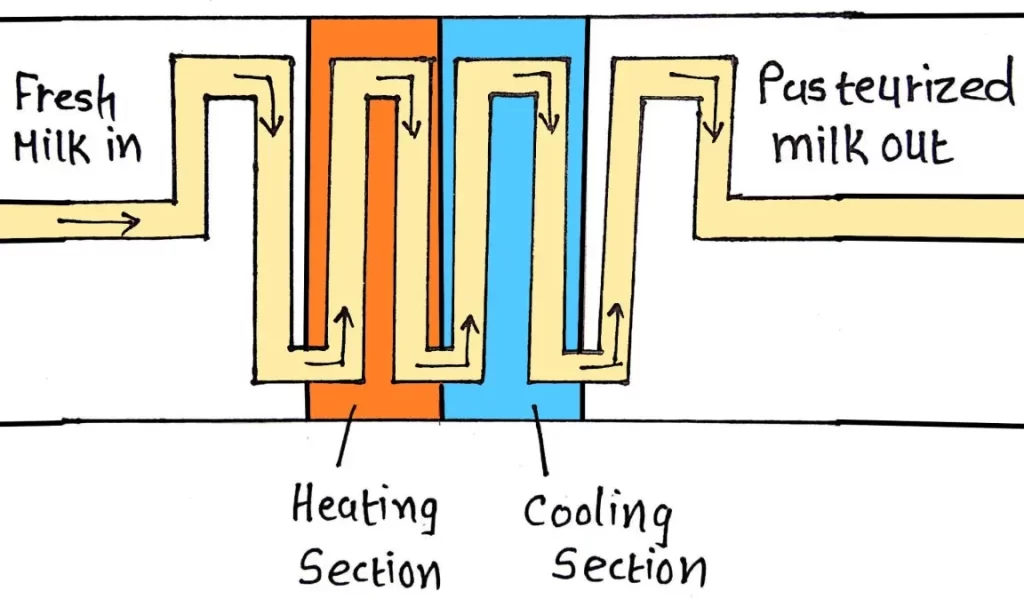
Louis Pasteur invented the method of pasteurization in order to prevent decaying of beer and wine.
He provided mild heating, which was adequate enough to kill the microbes that were causing the spoilage problem.
At the same time, taste of product didn’t change.
The same principle was applied to milk and its products which is known as pasteurization.
Definition
Pasteurization is the treatment for eliminating harmful pathogens from milk, yogurt, ice-cream, fruit juice, beer and other packaged food (specially liquids).
Types
- Low Temperature Hold method (LTH)– Providing of 63°C for 30 minutes before cooling to 7°C.
- High Temperature Short Time (HTST)/ Flash Pasteurization– Providing 72°C for at least 15 seconds before cooling to 10°C.
Milk can be stored in refrigerator for prolonged time.
- Ultra-high Temperature (UHT)- After reaching 140°C for 4 seconds, fluid is cooled rapidly in a vacuum chamber.
Then milk or juice are packaged in an airtight container.
All the microorganisms gets killed so, products can be stored for several months without refrigeration.
UHT treated products are used in Europe, less developed countries or areas where refrigerators are not available.
How to test that the product is effectively sterilized by pasteurization?
Answer is Phosphatase activity test.
Phosphate is naturally found enzyme in milk which will be inactive in pasteurized products.
If it is found present, that suggests the inadequate treatment.
Advantages
- It lowers the number of microbes.
- So, milk can be preserved for long time under the refrigeration.
- All non-sporing microbes like Mycobacteria, Brucellae, Salmonella etc gets killed.
Limitations
- Bacteria which are heat-resistant (thermostatic) or in spore forms may survive.
- Example: Coxiella burnetii.
HOT AIR OVEN

Hot air oven is widely used for sterilization by dry heat.
This instrument is actually a heated chamber that allows air to circulate in gentle flow.
Heat does not penetrate materials inside easily. So, long period of exposure to high temperature is necessary.
Parts of the instrument
- Metallic chamber made up of stainless steel or aluminium.
- Outer case- Thick layer of glass fibre for insulation.
- Double walled door.
- Inner surface of door- Gasket made up of asbestos.
- Heating elements are fitted at the bottom of the chamber.
- Fan, thermometer and ventilator are also provided.
Procedure
- Materials to be sterilized are placed properly.
- Adjust the temperature to 150°C and ventilator is kept open until the temperature reaches to 115°C.
- Once desired temperature is achieved, door is closed to reach the temperature of 150°C.
- After 1 hour, oven is switched off and allowed to cool to about 60°C.
Mechanism of action
- Coagulation and oxidation of cellular proteins.
- Oven is heated by electricity.
- The heating coils in the sides or bottom of the chamber causes rise of hot air inside the chamber through natural convection (transmission).
- Heated air circulates throughout the chamber at a high velocity, causing rapid transfer of energy from the air to the instrument, that’s why it reduces the time required for sterilization.
- Power of heat penetration is low because hot air is a bad conductor of heat.
Precautions should be kept in mind
- Should not be overloaded.
- Material should be dried properly.
- Materials should be arranged in such a way that air can circulate freely inside the chamber.
- Test tubes, flask etc. should be fitted with cotton plugs.
- Paper should be wrapped around petri dishes and pipettes.
- Materials which are inflammable or made up of rubber should not be kept inside the chamber.
- Before opening the door of oven after work is done it must be allowed to cool for at least 2 hours. This is because glass ware may crack by sudden cooling of temperature.
Uses
- For sterilization of glassware like petri dishes, glass syringes, pipettes, test tubes and other laboratory equipments.
- Surgical instruments like scalpels, scissors, forceps etc.
- Chemicals like liquid paraffin, glycerol, fat, glove powder etc.
INCINERATION

Incineration is an excellent method for safe destroying of materials like contaminated cloths, carcasses (dead bodies), pathogenic materials, body organs, placenta etc.
- It is a dry oxidation process by high temperature which can reduce organic and burnable waste to inorganic non-burnable matter.
- Materials are reduced to ashes by burning.
- It can cause very significant reduction in weight and volume of waste.
- Suitable to process wastes that cannot be recycled, reused or disposed of in a land.
Wastes that are not be incinerated are:
- Sealed ampoules or those having heavy metals.
- Reactive chemical wastes.
- Plastics with PVC.
- Pressurized gas containers.
- Silver salts and radiographic wastes.
- Broken thermometers, used batteries, lead-lined wooden panels etc.
Types of Incinerators
- Double-chamber pyrolytic incinerators- Designed to burn infectious health care-wastes.
- Single-chamber furnaces with static grate- Not recommended to process biological wastes.
- Rotary kilns operating at high temperature- Can decompose genotoxic substances and heat resistant chemicals.
Advantages- Volume of waste materials decrease up to 90%.
Disadvantages- Total destruction, high construction but costly.
AUTOCLAVE
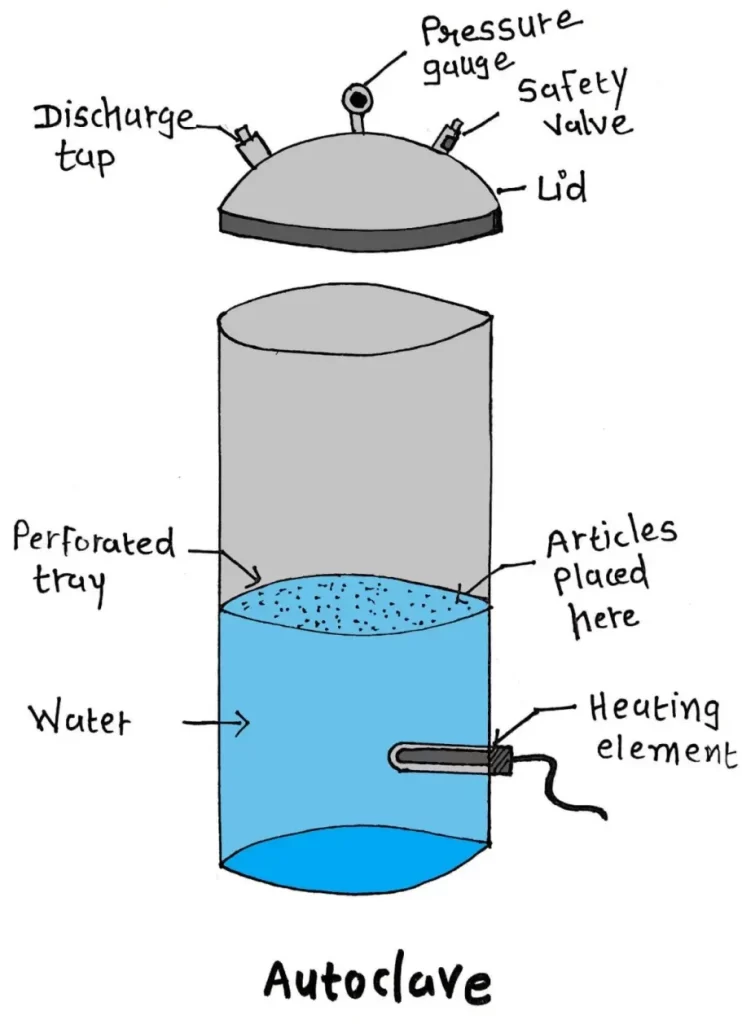
Autoclave is an instrument used in laboratories and hospitals to sterilize equipments.
Auto means self and clavis means key. Autoclave is a Latin word which means “Self-locking device”.
Its basic function is similar to pressure cooker which we use in our kitchen.
In the year 1879 Charles Chamberland invented the first pressure cooker.
Autoclave uses the high pressure and steam in combination to transfer the heat to the items placed inside the chamber which denatures the bacterial proteins.
Principle
- Water boils when the pressure of its vapour gets equal to the surrounding atmosphere.
- Steam contains higher energy.
- Autoclave provides pressurized saturated steam in the chamber in a controlled manner.
When pressure of gas increases, the temperature of gas also increases equally.
Parts of autoclave
Made up of mainly 3 parts-1) Pressure chamber; 2) A Lid; 3) Electric heater.
- PRESSURE CHAMBER– Large cylinder made up of gunmetal or stainless steel in which sterilizing material is placed.
It contains a compartment for water known as Steam Jacket.
- A LID– It is sealed by clamps and made airtight with chamber.
It is provided with a discharge tap, a pressure gauge (to regulate pressure) and a safety valve (to remove extra steam).
- ELECTRIC HEATER– It is attached with steam jacket which heats the water to produce steam.
Procedure
- Set up- Water is filled in the cylinder.
Sterilizing material is placed inside the pressure chamber.
Lid is closed and electric heater is put on.
Suitable pressure is adjusted by safety valve.
- Steam flows into sterilizing chamber from steam jacket.
- Cold air is forced out.
- Pressure increased by 15 pounds/square inch with the help of valves.
- Temperature rises to 121°C for 15 minutes.
- The superheated water molecules rapidly conduct the heat into microorganisms.
- For dense objects, up to 30 minutes exposure is required.
Different type of autoclaves
Many types are available.
- Gravity displacement is most common type used in laboratories.
- Positive pressure displacement type.
- Negative pressure/ vacuum displacement type.
- Cold sterilization autoclaves.
- Stove top autoclaves.
- Gas autoclaves.
- Ultraviolet autoclaves.
Uses of autoclave
- To prepare materials for bacteriological cell cultures with no contamination.
- To sterilize contaminated materials.
Advantages
- Microorganisms can be killed within short period of time due to high pressure steam.
Disadvantages
- Autoclaves cannot be used for the materials which cannot tolerate 115°C temperature.
Example: Plastic ware, sharp equipments becomes dull.
