There are about 30 species of Genus Staphylococcus that have been identified.
Out of them 14 species are associated with humans and animals.
In 1878, Robert Koch was the first person who identified them in pus.
In 1880, Louis Pasteur cultivated them for the first time.
GENERAL CHARACTERISTICS
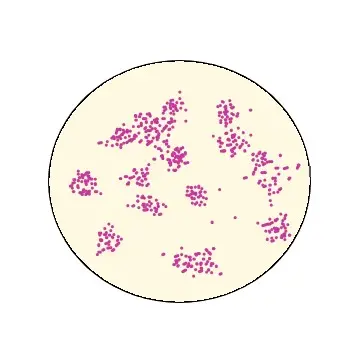
- Gram positive cocci, ovoid or spherical in shape.
- Non-motile.
- Arranged in groups.
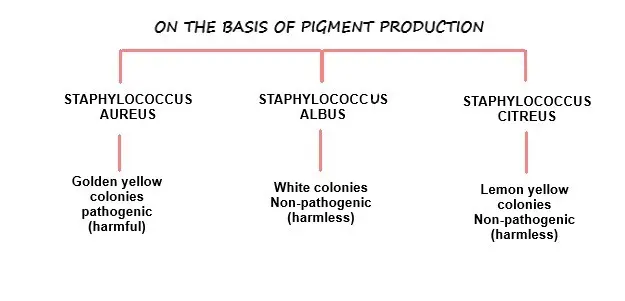
- They form white, yellow or golden yellow coloured colonies on nutrient agar.
- Capacity of haemolysis is variable.
- Pathogenic stains (sub types) can ferment sugar, produce acid, liquefy gelatin, produce coagulase and produce pus in wound.
Table of Contents
ToggleSTAPHYLOCOCCUS CLASSIFICATION
STAPHYLOCOCCUS AUREUS (STAPHYLOCOCCUS PYOGENES)
INTRODUCTION
Staphyle- Bunch of grapes
Kokkos- Berry
Aureus- Golden
This name is given due to its yellow pigmented colonies.
MORPHOLOGY
- They are ovoid or spherical in shape.
- Size- 0.8 to 0.9 µm.
- They are non-motile, rarely having capsules, non-spore forming species.
- They are gram positive bacteria.
- Arrangement- They are arranged in grape like clusters/groups (because cell division occurs along multiple axis and so, generating irregular, grape like clusters of cells).
CULTURAL CHARACTERISTICS
- Aerobic or facultative anaerobes.
- Required optimum temperature to grow is 37°C (range from 10°C-45°C).
- They are non-fastidious organisms which means they can grow in ordinary media (that does not contain blood).
- Colonies in solid media are round, smooth, raised and glistening.
- They can produce catalase.
- They are resistant to drying, heating, and 9% Nacl, but easily inhibited by 3% hexachlorophene.
BIOCHEMICAL REACTIONS
- Fermentation of glucose produces mainly lactic acid.
- They also can ferment mannitol.
ANTIGENIC STRUCTURE
- They have specific antigens on the cell wall.
- They contain both the antigenic polysaccharide and proteins that help in grouping of strains to a limited extent.
- Peptidoglycan which is the exoskeleton of cell wall, provides rigidity. This layer is important in the pathogenesis of infection because-
- It induces cytokines and opsonic antibodies (can enhance phagocytosis) production.
- It can attract polymorphonuclear leukocytes.
- It activates complement.
- Teichoic acid linked to this peptidoglycan layer can work as antigens.
- Protein A which is a cell wall component can freely combine with specific antigen.It involves in co-agglutination and interferes with phagocytosis and damage to platelets.
HABITAT AND TRANSMISSION
- Their main habitat is human nasal mucosa, skin, axilla or perineum.
- They get transmitted from person to person through direct contact or exposure to contaminated materials (bad linens, clothing, utensils etc).
- They also get transmitted via oral secretions or spread via bloodstream.
- Transmission through food is also a common occurrence.
PATHOGENESIS
Staphylococcus aureus can produce disease because,
- They can adhere to the cells.
- They can spread in tissues and form abscesses, produce extracellular enzymes and endotoxins.
Factors that promote the pathogenesis
- Structural components- Capsule, Peptidoglycan, Teichoic acid, Protein A.
- Toxins- Cytotoxins, Endotoxins (Enterotoxins, Exfoliative toxins, TSST).
- Enzymes- Coagulase, Catalase, Hyaluronidase, Beta lactamase, Degradative enzymes.
Structural components
- Capsule
- Capsule inhibits the chemotaxis and phagocytosis process.
- They facilitate the attachment to catheters and other synthetic materials.
- Peptidoglycan
- This layer provides osmotic stability.
- This stimulates endogenous pyrogen production.
- Inhibits the process of phagocytosis.
- Stimulates abscess formation (by attracting leukocytes).
- Teichoic acid
- This regulates concentration of cations near cell membrane.
- Acts as a mediator for adherence of organisms to mucosal cells.
- Protein A
- It binds to Fc protein of IgG at the complement binding site and prevents the activation of complement.
Toxins
- Cytotoxins
- These toxins damage the cell membranes.
- Examples- alpha, beta, delta, gamma, leucocidin.
- Exotoxins-
There are mainly three exotoxins which are clinically important.
Enterotoxins
- Heat stable (resistant to 100°C for 30 mins).
- They cannot be neutralized by digestive enzymes of gastro-intestinal tract.
- They can cause food poisoning.
Exfoliative toxins–
- It is a protease (enzyme that can break down the protein in smaller pieces) which can split the intercellular junction that cause epidermolysis.
- This protease affect GM4-glycolipids which are more in children in compare to adults.
- That is why these toxins cause scalded skin syndrome (desquamation/peeling of skin) in children.
Toxic shock syndrome toxin (TSST)–
- These toxins stimulate many helper T cells to release large amount of lymphokines.
- This causes toxic shock syndrome in mainly women having menstruation, using tampons or individuals with wound infection.
Enzymes
- Coagulase– They cover the infection by formation of fibrin layer around the abscess.
- Catalase– They inhibit phagocytosis.
- Hyaluronidases– Acts as a spreading to antibiotics.
- Beta lactamase– Causes resistance to antibiotics.
- Degenerative enzymes– These promote the destruction of tissues and spread of bacterial infection.
DISEASES CAUSED BY STAPHYLOCOCCUS AUREUS
The clinical manifestations caused by staphylococcus aureus can be classified into mainly two groups,
- Inflammatory diseases
- Toxin mediated diseases
Inflammatory diseases
- Skin infections– Boils, Carbuncles, Stye, Mastitis, Folliculitis, Impetigo, Furuncle, Cellulitis, Abscess formation etc.
- Systemic diseases– Osteomyelitis, Septic arthritis, Endocarditis, Meningitis, Broncho-pneumonia, Empyema etc.
- Septicaemia– Commonly occurs due to outbreaks of hospital wound infection.
Toxin mediated diseases
- Food poisoning-
- Causes- Ingestion of contaminated food (with preformed enterotoxin) that is improperly cooked and kept unrefrigerated for hours.
- Types of food- Carbohydrate rich food like Cakes, Pastry, Milk etc.
- Transmission via- Hands or Nose of cook, Food handlers, Carriers.
- Incubation period- 1-8 hours after ingestion of food.
- Signs and symptoms- Nausea, Vomiting, Diarrhoea and General malaise without food.
- Toxic shock syndrome (TSS)-
- Causes- Strain of staphylococcus aureus containing TSST-1 gene.
- Common occurrence-Use of tampons which facilitate growth of staphylococcus aureus and TSST-1 production. This toxin is absorbed from vagina and then circulates in blood which causes systemic effects.Also occurs with patients having wounds or localized infections.
- Sign and symptoms- Acute onset of fever, vomiting, diarrhoea, muscle ache and rashes over the body.
- Complications- Hypotension, cardiac or renal failure.
- Staphylococcal scalded skin syndrome (SSSS)-
- Causes- Exfoliative toxin produced by phage 2 strains of s. aureus.
- Common occurrence- Babies and young children.
- Sign and symptoms- Large areas of pilled skin (desquamated) with generalized bullae formation (fluid filled sac).
LABORATORY DIAGNOSIS
- Specimens- Pus, sputa, CSF, Blood, Urine etc.
- Gram staining smears- Presence of Gram-positive cocci in groups.
- Cultural findings-
- Usually large, smooth and translucent (semi-transparent) colonies are found.
- These colonies show complete haemolysis on blood agar. While on nutrient agar they show golden yellow or white coloured appearance.
- Mannitol salt agar- Used for staphylococcal food poisoning cases as differential and selective medium.
- Isolated colonies can be identified by Catalase test, Coagulase test, Phage typing etc.
TREATMENT
- Several antibiotics are effective against staphylococcus. Example- Erythromycin, Tetracyclines, Ampicillin, Cephalosporins.
- Staphylococcus aureus are remarkably able to develop resistance to antibiotics especially in hospital strains.
- About 80% of hospital strains staphylococcus are resistant to penicillin (Beta lactamase of enzyme produced by them breaks down the lactam ring in penicillin and cephalosporins).
ANTIBIOTICS
- Penicillin or Cephalosporin- For non-resistant (sensitive) organisms.
- Rifampicin, Quinolone, Clindamycin etc.
- Some combinations like Amoxicillin and Augmentin.
I hope this article has given you a clear understanding of the Genus Staphylococcus. Feel free to share it with your friends so they can also benefit from this information! 😊
