
Here is a practical method of Erythrocyte Sedimentation Rate (ESR) which is a valuable test to detect the presence of inflammation in the body.
This test is measurement of the rate at which the red blood cells of a blood sample settles down in a vertical narrow-graduated glass tube (Westergren’s pipette or Wintrobe’s tube/Haematocrit tube) (usually in one hour).
This test is an easy to perform, widely used and less expensive.
STUDENT OBJECTIVES
At the end of the practical, you should be able to:
- Understand the clinical importance of ESR.
- Describe the reason of red blood cells settling down in a tube.
- Know the factors that affect the sedimentation rate of RBCs.
- What are the sources of errors and what precautions can be taken?
- Remember the various physiological and pathological conditions in which ESR gets increased or decreased.
Table of Contents
ToggleWhy this test is known as Erythrocyte Sedimentation Rate?
To understand this, you need to know about the suspension stability of red blood cells.
- Blood is a colloid in which RBCs (Red Blood Cells) are suspended.
- In normal condition, the RBCs and plasma do not separate out because blood keeps mixing continuously (due to circulation).
- When blood is drawn out of the body, blood cells do not separate out easily due to its viscosity.
- To find out the suspension stability of RBCs the blood is made to stand in a column without disturbing.
- So, it will leave clear fluid on top which is known as supernatant that is equal to plasma.
- Supernatant is separated because RBCs settle down or we can say sediments so, this test is known as Erythrocyte Sedimentation Rate.
It might have come in your mind that,
Why RBCs settle down?
Two reasons are there which are responsible,
- Forces that pull the RBCs to settle down: Weight to surface ratio and downward Gravitational force.
- The factor that does not allow RBCs to settle down and pushes up: Viscosity of plasma (If the fluid is thicker, the object do not settle down).
So, the push and pull factors decides the suspension stability or Sedimentation Rate of Red Blood cells.
(Example: Imagine the viscosity of following fluids in increasing order. PETROL—KEROSINE—WATER—OIL—MERCURY)
PRINCIPLE OF ESR
In the circulating blood the red cells remain uniformly suspended in the plasma.
However, when a sample of blood to which an anti-coagulant has been added, is allowed to stand in a narrow vertical tube.
The red cells being heavier than colloid plasma, settle or sediment gradually towards bottom of the tube.
The rate at which red cells sediment is called as Erythrocyte Sedimentation Rate which is recorded at the end of one hour in millimetre.
TRADITIONALLY THERE ARE TWO METHODS
- Westergren’s method
- Wintrobe’s method
INSTRUMENTS REQUIRED
- Westergren’s pipette (for Westergren’s method)
- Wintrobe’s tube (for Wintrobe’s method)
- Pasteur pipette
- Westergren pipette stand/ Wintrobe tube stand
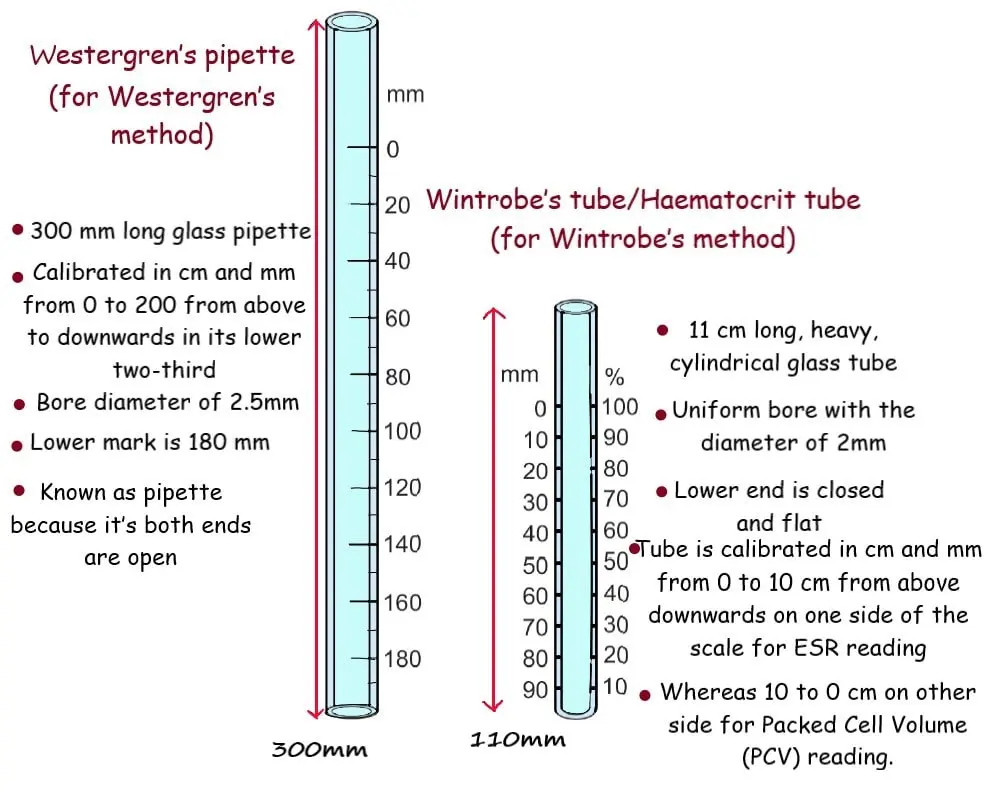
Westergren’s pipette (for Westergren’s method)
- It’s 300 mm long glass pipette with a bore diameter of5mm.
- It is calibrated in cm and mm from 0 to 200 from above to downwards in its lower two-third.
- Lower mark is 180 mm.
- It is known as pipette because it’s both ends are open.
- The higher sensitivity and the long tube are particularly important in cases where ESR is high (>80).
- Blood sample is venous blood using trisodium Citrate (3.8%) as an anti-coagulant.
Wintrobe’s tube/Haematocrit tube (for Wintrobe’s method)
- It is 11 cm long, heavy, cylindrical glass tube.
- It has uniform bore with the diameter of 2mm.
- Its lower end is closed and flat.
- The tube is calibrated in cm and mm from 0 to 10 cm from above downwards on one side of the scale for ESR reading.
- Whereas 10 to 0 cm on other side for Packed Cell Volume (PCV) reading.
- Blood sample is venous blood using Ethylene diamine tetra acetic acid (EDTA) as an anti-coagulant.
Pasteur pipette
- It is 8-10-inch glass tube drawn to a long thin nozzle with a rubber teat.
- Nozzle is about 14 cm long.
- Rubber teat is used to suck blood into pipette by a slight pressure.
- It is used for filling the Wintrobe tube.
Westergren pipette stand
- Commonly used Westergren stand can accommodate up to 6 tubes at a time.
- For each pipette there is a screw cap that slips over its top and at its lower end, the pipette presses into a rubber pad or cushion.
- When the pipette is fixed in position, there is enough pressure of screw cap is applied to prevent leakage of blood from its lower end.
- This stand ensures the vertical position of pipette.
Wintrobe tube stand
- It is a vertical stand that holds tube in vertical and motionless position.
- Commonly used Wintrobe stand can hold up to 3 (or 6) tubes at a time.
REQUIRED BLOOD SAMPLE
A vial of venous blood (2ml) using an Anti-coagulant.
Blood should be collected in fasting hours.
Blood sample should be used within 2 hours of collection.
METHOD OF ESR
- Draw 2ml of blood sample from the vein of your subject.
- Transfer it into a vial containing an anti-coagulant.
- Mix them by inverting or swirling the vial after applying the cap (Do not shake because it will cause frothing and rupture of RBCs). Or you can gently rotate the sample between the palm of your hands in order to mix the blood thoroughly.
- Examine your collected blood sample and confirm the absence of clot in it. The tube/pipette should be dry and clean.
- Fill the Westergren’s pipette by sucking up to zero mark. Bring the blood column to exact zero mark after placing your finger tip over the top of pipette to control the flow of draining blood. (In case of Wintrobe tube, Pasteur pipette is used to fill the column).
- Slow drainage is necessary because, the blood sticking around the internal surface will later come down and raise the level of reading.
- Clean the outer surface of pipette.
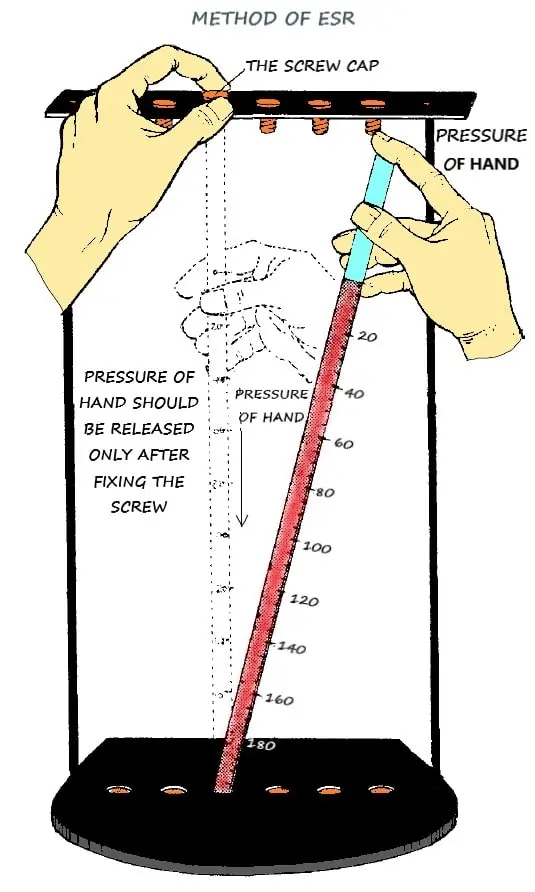
- Now, by closing the upper end of pipette with the tip of your finger transfer it to the Westergren’s stand. Firmly press the lower end of pipette into the rubber cushion. Take care that no blood should be escaped.
- Slip the upper end of pipette under the screw cap.
- Release the pressure of your finger tip only after securely fixing of screw cap.
- Fix the pipette exactly vertical.
- Observe any change in blood level from the zero mark. If it is raised above, bring it to zero by reducing the pressure of screw cap. If it has fallen down, some blood must have escaped. So, refill the pipette again by taking it out and fix it properly in the stand.
- Keep this sample in standing position and undisturbed for one hour.
- Read the upper level of red column at the end of one hour. Above the red column there will be clear plasma or supernatant.
- Readings from Wintrobe’s tube and Westergren’s pipette will be different.
- Express your reading as ………… mm 1st
- Also record the room temperature.
Note: The result is not expressed as …………mm per hour. Do not take half hour reading and then double it to arrive at 1 hour.
PROCESS OF SEDIMENTATION
What happens during this hour?
Let’s understand the process of sedimentation in three phases.
1. Phase of Initial fall
- It is of about 10-15 minutes.
- A little separation is observed.
- Weight to surface ration of RBCs causes little fall.
2. Phase of Rapid fall
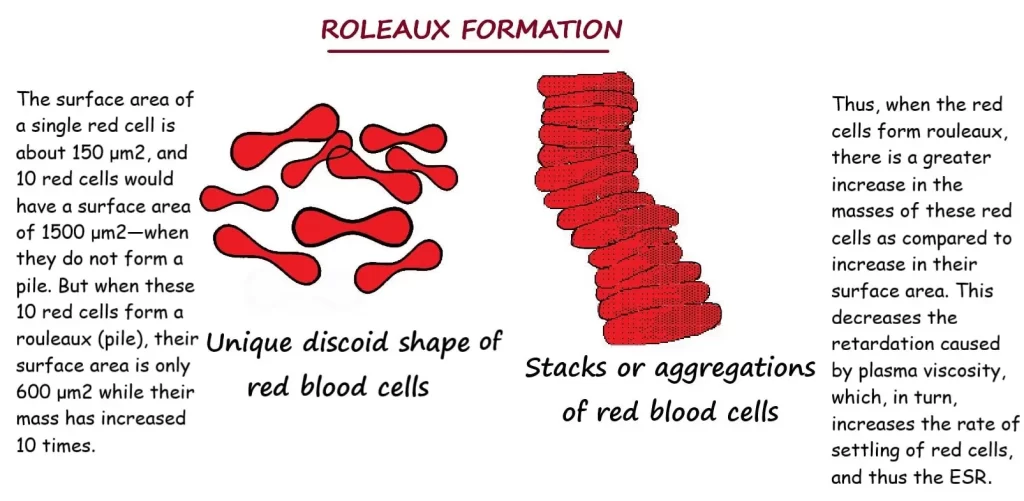
- This phase lasts for 40- 45 minutes.
- Rouleaux formation is completed and RBCs comes into pile formation.
- Individual RBC is exposed to all the surfaces.
- Now when they are arranged in Rouleaux formation, only one side surface of upper and lower surface of RBCs along with side surface of all RBCs are exposed.
- So, the effective surface for remaining floating decreases tremendously in relation to weight.
- At this point surface to weight ratio becomes favourable to sedimentation.
- Even in viscous plasma the RBCs sediments rapidly.
3. Packing phase
- During rapid fall, the sedimentation leaves gape in between RBCs.
- In this phase, packing is observed.
- So, there is little fall of blood cells.
- This stage lasts for 10-12 minutes.
OBSERVATIONS
- The observations should be carried out between 22-27°C. the standard reading can not be achieved if the room temperature goes beyond these range.
- If there is no haemolysis, there should be a sharp demarcation line between the red cells and clear, cell-free, straw coloured plasma.
INFERENCE
- Increase in ESR indicates the fast Rouleaux formation that is caused by a peculiar pattern of plasma molecule.
- This peculiar pattern suggests the presence of some disease in the body.
- But it can not indicate the nature of disease.
- So, two or more consecutive reading at definite interval with the increased ESR confirms the continuous or increased activity of diseased process. Where as a decrease in ESR suggests the arrest of the process.
This is how, changes in the ESR are more important than the actual rate observed by any of the two methods.
FACTORS AFFECTING ESR
- Red blood cells having high specific gravity settles down in plasma which have low specific gravity.
- Low viscosity of plasma increases the rate of sedimentation.
- Increase in the size of red blood cells causes increase in ESR.
- Clumping of cells increases sedimentation rate.
- ESR reduces in case of spherocytosis as it prevents Rouleaux formation.
- Rise of temperature causes increase in ESR.
- Increased Red blood cells count decreases ESR.
- ESR gets decreased with increase in plasma lecithin and albumin.
- ESR gets increased with increase in fibrinogen
MECHANICAL FACTORS AFFECTING ESR
- It is necessary to keep the ESR tube exactly vertical. A tilt of 30 degrees can cause errors up to 30%.
- The Stand/Rack holding the tubes must not subject to any movement or vibrations.
- With the increase of temperature, the sedimentation rate increases.
- ESR tubes which are narrow than the standard bore size will give lower sedimentation rate as a result.
SOURCES OF ERROR
- Improper ratio of blood and anticoagulant
- Haemolysed (ruptured red blood cells) sample of blood
- Clotted blood sample
- Presence of air bubbles in the sample
- Delay in performing the test
- Errors due to sunlight, small sized bore of the tube, dirty or wet tube
Can we use oxalate mixture in Westergren’s method and sodium citrate in Wintrobe method?
No. these anticoagulants cannot be interchanged. If we use sodium citrate in Wintrobe method, the blood will be diluted too much in compare to the height of the tube that will give the false ESR value.
Why the reading of ESR is taken after one hour?
Because up to 95-98% of red blood cells gets settle down by the end of an hour. After one hour the ESR is not significantly affected by sedimentation.
What are the clinical importance of ESR?
- As an indicator of body’s reaction to tissue injury or inflammation.
- ESR values are not diagnostic.
- They will not tell the name of the disease that is causing a raised ESR.
- It does not tell you exactly where the inflammation is located in body.
- It is a sensitive indicator of tissue damage.
- ESR is a valuable prognostic tool in the course of diseases like tuberculosis, rheumatoid arthritis etc.
- Weekly ESR results of a patient under treatment, If ESR tend to decrease- suggests improvement. If ESR tend to increase- suggests deterioration in disease.
What are the physiological variations of ESR?
- AGE: Low in infants due to polycythemia that gradually increases to adult range in following few years.
- SEX: Higher in females, especially while menstruation.
- PREGNANCY: ESR begins to increase after 3rd month of pregnancy which returns to normal after delivery in a few weeks.
- PEOPLE LIVING AT HIGH ALTITUDE: Relatively higher ESR.
- BODY TEMPERATURE: ESR varies with temperature within limit.
What are the pathological variations of ESR?
Pathological increase
- All acute or chronic infections.
- Anaemias (except spherocytosis, sickle cell and pernicious).
- Bone diseases
- Connective tissue disorders
- All malignant diseases
- Acute inflammations
- Nephrosis
- Trauma
- Surgery
Pathological decrease
- Polycythemia
- Anaemias
- Afibrinogenemia
- Severe allergic reactions
